Appendicitis, a medical urgency demanding immediate attention, unveils itself through seemingly innocuous symptoms that can rapidly evolve into a life-threatening situation. This comprehensive blog aims to demystify the complexities associated with appendicitis. From understanding its fundamental aspects and identifying appendicitis symptoms to exploring the various stages, diagnosis methods, and specialized considerations for children, we embark on a thorough journey. Recognizing the critical role of prompt medical attention, this guide equips you with essential insights to navigate the intricate landscape of appendicitis, ensuring a comprehensive understanding of this potentially serious medical condition.
Overview of Appendicitis
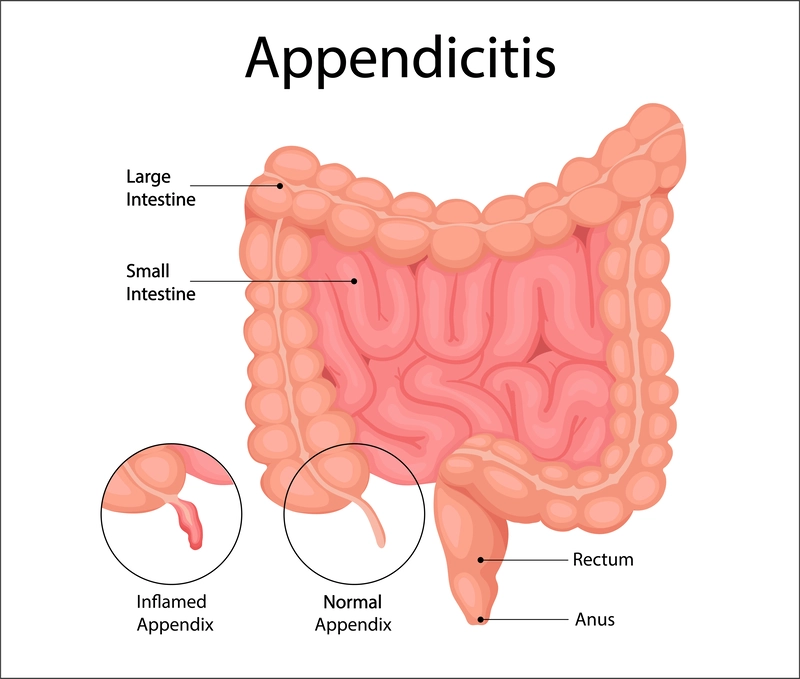
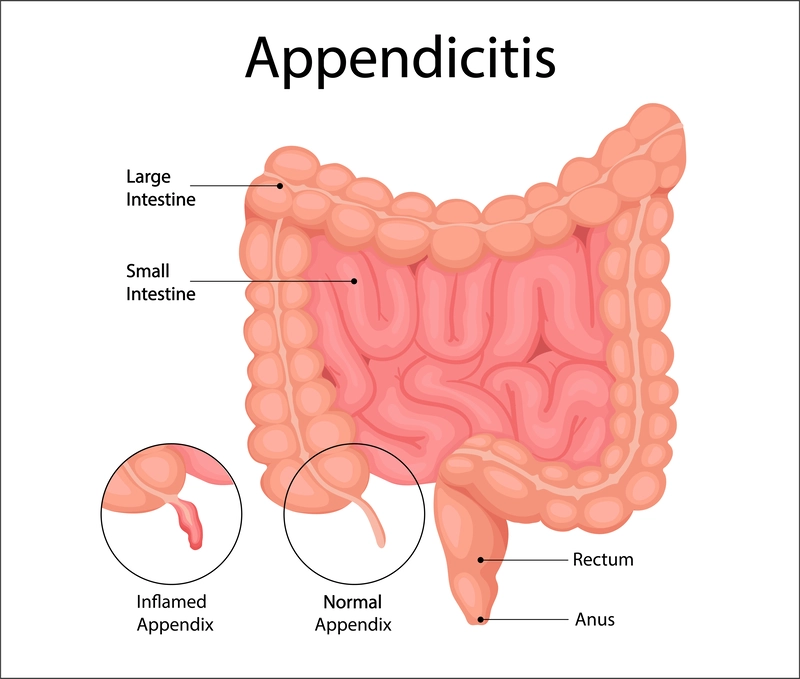
Appendicitis is a medical condition characterized by the inflammation of the appendix, a small, tubular pouch located at the lower right end of the large intestine. This inflammation often results in sudden and intense pain in the lower abdomen. The appendix, about the size of a finger, can become obstructed or infected by the movement of feces through the large intestine. As a consequence, the appendix swells, and in severe cases, it may even burst, posing a significant medical emergency. A ruptured appendix releases bacteria from the bowels into the abdominal cavity, causing a condition known as peritonitis. This infection can further extend to the bloodstream, leading to life-threatening complications such as sepsis. Due to the potential risks associated with a burst appendix, the standard and most effective treatment for appendicitis is surgical removal of the appendix, a procedure known as appendectomy. It is essential to note that the appendix is considered a non-essential organ, and its removal does not significantly impact the body's normal functioning. Despite its seemingly minor role, prompt medical attention and intervention are crucial in managing appendicitis to prevent complications and ensure the well-being of the affected individual.
Types of Appendicitis: Acute appendicitis vs. chronic appendicitis?
The classification of appendicitis into acute and chronic forms highlights distinct patterns of onset and progression in this medical condition. Acute appendicitis is the more prevalent and well-understood form, characterized by a sudden onset of symptoms that rapidly worsen. This acute condition is widely recognized and constitutes the majority of appendicitis cases. Acute appendicitis is the predominant form of appendicitis and exhibits a higher incidence, particularly among specific age groups. The prevalence of acute appendicitis is notably significant between the ages of 10 and 30, with a peak occurrence during the teen years. However, it is essential to note that even younger children can experience this condition. In the United States, statistics indicate that approximately 5% of the population will encounter acute appendicitis at some point in their lives. This underscores its significance as a prevalent abdominal ailment, and it stands out as the leading cause of abdominal pain necessitating emergency abdominal surgery. The need for prompt medical intervention in cases of acute appendicitis is further emphasized by its potential to lead to serious complications, including a ruptured appendix.
Chronic appendicitis is comparatively rarer, occurring in approximately 1% of the population. Chronic appendicitis is believed to manifest when the appendix undergoes intermittent irritation over an extended period without a significant deterioration in symptoms. Unlike acute appendicitis, the symptoms of chronic appendicitis may not escalate dramatically, potentially leading to its underrecognition. Despite its less pronounced symptomatology, it is crucial to emphasize that any form of appendicitis is a serious medical concern. One notable challenge in diagnosing chronic appendicitis lies in its subtle and intermittent nature, making it imperative for individuals experiencing chronic abdominal pain of unknown origin to seek medical attention. The symptoms of chronic appendicitis may not follow the acute trajectory typical of its counterpart, but the risk of escalation remains. Given the potential for chronic appendicitis to evolve into an acute state at any time, healthcare professionals typically adopt a standardized approach to its management. Timely medical evaluation and intervention are paramount to ensure accurate diagnosis, appropriate treatment, and the prevention of complications.
What does Appendicitis feel like? Common Signs and Symptoms of Appendicitis
Appendicitis manifests through a range of symptoms, although not everyone experiences the same set of indications. However, only about half of individuals with appendicitis exhibit the classic presentation of symptoms, making diagnosis sometimes challenging. Certain demographics, such as children, elderly adults, and pregnant individuals, may be less likely to display the typical signs.
Abdominal Pain: In the typical scenario, abdominal pain initiates in the middle of the abdomen, near the belly button, and may persist or come and go for several hours. As time progresses, the abdominal pain intensifies, accompanied by nausea and vomiting. After a few hours, the nausea typically subsides, and the pain shifts to the lower right abdomen, the location of the appendix. At this stage, the appendicitis pain becomes more focused and continues to escalate.
Nausea and Vomiting: As appendicitis progresses, a sense of nausea tends to ensue, often culminating in vomiting. The digestive system becomes disrupted due to the inflammation, leading to a feeling of queasiness. Persistent nausea, particularly when coupled with other appendicitis symptoms, serves as a red flag for potential appendicitis.
Loss of Appetite: A sudden and unexplained loss of appetite frequently accompanies appendicitis. Individuals may find themselves disinterested in food or experience a notable decrease in their usual dietary intake. This diminished appetite reflects the body's response to the inflammatory process within the appendix.
Fever: A low-grade fever is a common development, with up to 40% of individuals experiencing increased body temperature. This may indicate an elevated immune response, heightened inflammation, or the spread of infection.
Malaise: A general feeling of malaise may also be present, characterized by a lack of energy, motivation, and an inclination to rest.
Abdominal Swelling and Tenderness: The affected individual may notice swelling in the abdominal region, and gentle pressure or palpation may elicit tenderness. Abdominal swelling indicates the inflammatory process at play, and tenderness provides additional diagnostic clues for healthcare professionals.
Urinary Symptoms: They may manifest as a sensation of increased urgency or frequency resulting from appendicitis irritating nerves connected to the bladder.
Bowel Paralysis: This is another possible complication, temporarily halting bowel movements due to redirected blood flow to the appendix. This can lead to constipation and a sense of being unable to pass gas.
Diarrhea: Some individuals may experience diarrhea, reflecting overactive bowels due to inflammation affecting the adjacent end portion of the colon.
Given the variability in symptom presentation, it is crucial to seek prompt medical attention if appendicitis is suspected, especially when symptoms align with the classic pattern or if there are additional signs of complications. Early diagnosis and intervention are vital for effective treatment and prevention of serious complications, such as a ruptured appendix.
What causes Appendicitis?
Appendicitis can occur due to various factors that lead to inflammation, swelling, obstruction, and infection in the appendix. The size and location of the appendix make it susceptible to clogging and infection. Here are common causes and contributing factors to appendicitis:
Appendix Stones: Hardened fecal deposits, known as fecaliths or appendix stones, can block the opening of the appendix. These calcified deposits can carry bacteria and trap existing bacteria, leading to infection.
Lymphoid Hyperplasia: Swelling of the lymphoid tissue in the appendix, part of the immune system, can occur due to an infection elsewhere in the body. The swollen tissue may obstruct the appendix and contribute to infection.
Colitis: Inflammation in the colon resulting from infection or inflammatory bowel disease can affect the appendix. The infection may spread, or the inflammation itself may irritate the appendix.
Genetics: While appendicitis itself is not directly inherited, having a family history of appendicitis appears to increase the risk of developing the condition. The specific genetic factors involved in this association are not fully understood.
Physiological Stress: Severe physiological stress from critical illness can cause a temporary reduction of blood flow to the intestines, known as bowel ischemia. In rare cases, ischemic colitis may affect the appendix.
Foreign Objects: Some reports suggest that undigested seeds or nuts may get stuck in the opening to the appendix, causing inflammation. Generally, however, a high-fiber diet is associated with a reduced risk of appendicitis. Maintaining a balanced diet with an adequate intake of fiber, staying hydrated, and practicing good hygiene can contribute to overall digestive health and may help reduce the risk of certain gastrointestinal issues, including constipation-related problems that could contribute to appendicitis.
Other Factors: Tumors, parasites, and cystic fibrosis are among the factors that can block the opening to the appendix, leading to inflammation and infection.
It's important to note that appendicitis is a complex condition, and multiple factors may contribute to its development. While certain risk factors, such as family history, can increase the likelihood of appendicitis, the exact interplay of genetic and environmental factors is not fully understood. Early recognition of appendicitis symptoms and prompt medical attention are crucial for the diagnosis and management of appendicitis, which often requires surgical intervention to remove the inflamed appendix.
The Stages of Appendicitis - Exploring Early, Progressive, and Perforated Stages
The stages of appendicitis can be broadly categorized into three main phases: early, progressive, and perforated.
Early Stage of Appendicitis: Appendicitis often begins with nonspecific symptoms, marking the early stage of the condition. Patients may experience abdominal discomfort, loss of appetite, and mild nausea. The pain is typically dull and may manifest around the navel or upper abdomen. Clinically, this stage can be challenging to diagnose, as the appendicitis symptoms can be mistaken for other gastrointestinal issues. Patients might not immediately recognize the severity of their condition, and the discomfort may last for a few hours to a day before progressing to more distinct symptoms.
Progressive Stage of Appendicitis: As appendicitis advances, symptoms become more pronounced and localized. The pain intensifies and shifts to the lower right side of the abdomen, often becoming sharp and severe. Accompanying this, patients may develop fever, experience vomiting, and notice changes in their bowel habits. During a physical examination, a healthcare professional may conduct tests such as rebound tenderness or the psoas sign to assess abdominal pain. Additionally, diagnostic imaging studies, like ultrasound or CT scans, may be employed to confirm the diagnosis. Depending on the individual case, this stage can persist for several hours to a day or longer.
Perforated Stage of Appendicitis: Failure to address appendicitis promptly can lead to a critical stage where the appendix ruptures or perforates. This results in the release of bacteria and inflammation into the abdominal cavity. Symptoms may temporarily alleviate due to the reduced pressure, but complications such as peritonitis (inflammation of the peritoneum) and abscess formation arise. Perforated appendicitis is a medical emergency necessitating immediate surgical intervention. The duration of this stage can range from 24 to 72 hours or longer after the initial onset of appendicitis symptoms. Recognizing and treating appendicitis before reaching this perforated stage is crucial to prevent severe complications and ensure a better prognosis.
When to Seek Medical Attention for Appendicitis?
Seeking immediate medical attention for appendicitis is crucial, as the condition can quickly escalate and lead to serious complications. If you experience any signs or symptoms of appendicitis, it is important to seek medical help without delay. Here are key indicators that should prompt you to seek immediate medical attention:
Abdominal Pain Located in the Lower Right Quadrant: Appendicitis often presents with pain that starts around the navel and then shifts to the lower right quadrant of the abdomen. If you experience persistent or worsening pain in this specific area, it could be indicative of appendicitis.
Worsening Abdominal Pain: If you have abdominal pain that is progressively getting worse over time, especially in conjunction with other symptoms, it may be a sign of advancing appendicitis. The intensity and persistence of the pain are key factors.
Abdominal Pain Accompanied by Nausea and/or Fever: The combination of abdominal pain along with nausea and fever is a common set of symptoms in appendicitis. If you experience these symptoms concurrently, it is essential to seek medical attention promptly.
Abdominal Tenderness and Sensitivity to Touch: If you notice tenderness and sensitivity to touch in the lower right quadrant of your abdomen, especially when pressure is applied, it may be indicative of appendicitis. This tenderness can be identified during a physical examination by a healthcare provider.
Appendicitis is considered a medical emergency, and time is of the essence in obtaining a timely diagnosis and appropriate treatment. If you suspect appendicitis or experience any of the mentioned appendicitis symptoms, do not delay seeking medical help. Visit the emergency room or contact your healthcare provider immediately for a thorough evaluation and diagnosis. Early intervention is crucial in preventing complications associated with appendicitis, including the risk of appendix rupture.
Where to Press to Check for Appendicitis?
Here are several signs and techniques that healthcare providers use to assess for appendicitis:
- McBurney's Sign: This involves checking for tenderness at McBurney's point, which is the most typical location of the appendix. Providers locate it by drawing a line from the ASIS (anterior superior iliac spine, the bony bump on your hip) to the belly button and measuring the distance. McBurney's point is approximately two inches along this line or one-third of the distance.
- Psoas Sign: This sign involves checking for irritation of the psoas muscle, which may occur if the appendix is located behind the colon. The healthcare provider may ask the individual to flex or extend their right hip and observe for pain. If flexing the hip relieves pain, it's referred to as the psoas sign. If rotating the hip inward causes pain, it's known as the obturator sign.
- Dunphy's Sign: Coughing can exacerbate the pain in appendicitis, and healthcare providers may use this sign to assess the severity of discomfort.
- Blumberg's Sign: This sign involves applying pressure to a sore area and assessing if the pain worsens upon release. This phenomenon is also known as rebound tenderness.
- Rovsing's Sign: Applying pressure on the lower left side of the abdomen may produce pain on the lower right side, indicating potential appendicitis.
How to Check for Appendicitis at Home?
While the signs mentioned above are commonly used by healthcare providers, it's crucial to note that diagnosing appendicitis at home is challenging and not recommended. Although having an awareness of the techniques mentioned and an understanding of the appendicitis symptoms is beneficial, it's essential to emphasize that self-diagnosis and self-treatment should be avoided. If you, your child, or a loved one experiences symptoms such as persistent abdominal pain, fever, and other concerning symptoms that could be indicative of appendicitis, seeking medical attention is crucial. Medical professionals possess the expertise and tools to accurately diagnose and treat various conditions. Remember, while knowledge can be helpful for general awareness, it doesn't replace the need for professional medical assessment. If in doubt, it's always safer to seek prompt medical advice.
Diagnosis of Appendicitis: Techniques, Signs, and Imaging Insights
The diagnosis of appendicitis involves a combination of detailed questioning, a physical examination, and, if necessary, additional tests. Here is an overview of the diagnostic process for appendicitis:
Medical History and Physical Examination: A healthcare provider will ask you detailed questions about your symptoms, including the location and nature of the pain, the onset of symptoms, and any factors that worsen or alleviate the pain. They employ various signs and physical examination techniques to check for appendicitis, recognizing that symptoms can vary among individuals. One key indicator is the location of pain, particularly if it starts around the navel and then migrates to the lower right abdomen, following the typical pattern. However, it's important to note that some individuals may experience pain in different locations.
Blood Tests: Blood tests are commonly used to assess signs of inflammation and infection. Elevated levels of white blood cells (leukocytosis) and C-reactive protein (CRP) can indicate the presence of inflammation. These blood tests help support the diagnosis of appendicitis.
Imaging Tests: Imaging tests are crucial for visualizing the appendix and confirming the diagnosis. Common imaging modalities include:
Abdominal Ultrasound: This non-invasive test uses sound waves to create images of the abdominal area. It can help identify inflammation and swelling of the appendix.
CT Scan (Computed Tomography): A CT scan provides detailed cross-sectional images of the abdomen, helping to visualize the appendix and assess for signs of inflammation or other complications.
In some cases, healthcare providers may order additional tests to rule out other conditions that can present with similar symptoms. These may include pelvic exams for women, especially if gynecological conditions are suspected. It's important to note that not all cases of appendicitis follow the classic pattern, and additional tests may be necessary to confirm the diagnosis, especially if symptoms are atypical. Prompt diagnosis is crucial to initiate appropriate treatment, typically involving the surgical removal of the inflamed appendix (appendectomy) and to prevent the progression of complications associated with appendicitis.
Age-Related Challenges in Diagnosing Acute Appendicitis in Kids
Acute appendicitis, a common cause of emergency abdominal surgeries in both pediatric and adult populations, presents distinct challenges in young children. While it is relatively rare in neonates and infants, its occurrence increases in preschoolers, with rates varying among different studies. Notably, appendicitis progression appears more rapid in younger patients, suggested by variations in appendiceal development (the growth and maturation of the appendix). The thin-walled appendix and the underdeveloped omentum (a fold of peritoneum connecting the stomach with other abdominal organs) in infants may facilitate the swift spread of infection, leading to earlier perforation compared to adults. Young children's inability to articulate their symptoms complicates diagnosis, requiring caregivers to provide essential medical history.
Misdiagnosis is a prevalent concern, particularly in the youngest patients, with reported rates ranging from 9.1% to 16.9%. Gastroenteritis often masquerades as appendicitis in this age group. Delays in diagnosis correlate with patient age, emphasizing the need for vigilance, especially in infants and toddlers. Comparing symptoms across age groups reveals distinctions. Diarrhea and fever are more frequent in infants/toddlers than in preschoolers, while vomiting, respiratory symptoms, and diffuse abdominal pain are more common in those under five years old. Despite improvements in healthcare, perforated appendicitis remains a concern.
Laparoscopic appendectomy (A surgical procedure to remove the appendix using minimally invasive techniques), considered advantageous, may not fully mitigate postoperative complications. Complications, including intra-abdominal abscesses (collections of infected fluid within the abdominal cavity, a potential complication post-surgery), are more prevalent in younger patients, underscoring the importance of early diagnosis. Laboratory tests like ANC (Absolute Neutrophil Count) and WBC (White Blood Cell) count, while commonly used, show varying diagnostic performance across age groups. Ultrasound, gaining popularity, exhibits consistent diagnostic accuracy regardless of age.
Early ultrasound, coupled with clinical evaluation, emerges as a valuable tool in ensuring timely and accurate diagnoses, ultimately minimizing the risk of complications associated with appendicitis in young children.
Managing Appendicitis: The Crucial Role of Immediate Medical Intervention and Surgical Solutions
The management and treatment of appendicitis involve prompt medical attention and, in most cases, surgical intervention. While it is possible for appendicitis to spontaneously resolve if the cause, such as an obstruction, clears on its own, this is not common. Relying on spontaneous resolution is not recommended, and appendicitis is generally considered an emergency that requires immediate medical attention.
Appendicitis is treated as an emergency, and individuals with suspected appendicitis are typically evaluated and managed in the emergency room. The standard and most effective treatment for appendicitis is surgery, known as appendectomy. Antibiotics are an integral part of the treatment, addressing the infection associated with appendicitis. Surgery is usually performed within 24 hours of diagnosis to prevent the risk of appendix rupture. Almost everyone diagnosed with appendicitis will receive antibiotics. Antibiotic treatment is essential to address the infection and is often administered before surgery as a standard preventive measure. In very early and mild cases of appendicitis, healthcare providers might consider a wait-and-watch approach, using antibiotics alone to see if the condition improves. However, this approach is rare, as appendicitis often recurs if the appendix is not removed.
Surgical removal of the inflamed appendix, known as appendectomy, is the primary treatment. Surgeons often use minimally invasive methods, such as laparoscopic surgery, to perform the procedure. Given the urgency of appendicitis, surgery is usually scheduled within 24 hours of diagnosis to prevent complications. The appendix can rupture within 36 hours of the onset of symptoms. If complications arise during surgery, open abdominal surgery may be necessary. Surgeons will address and treat any complications that occur during the procedure. After surgery, the abdomen may be rinsed with a sterile solution to prevent infection. There are generally no significant side effects of having the appendix removed. While the function of the appendix is not entirely clear, it is considered to have a small role, possibly in the production of antibodies during childhood.
Progression of Appendicitis Complications: Recognizing the Urgency for Timely Intervention
Appendicitis, if not promptly treated, can lead to serious complications that progress in stages. These complications can have severe consequences, highlighting the importance of recognizing and addressing appendicitis as a medical emergency. The possible complications include:
Peritonitis and Spreading Infection: If the infection extends into the peritoneal cavity (peritonitis), it can spread to other organs and may enter the bloodstream, leading to septicemia. Infection in the bloodstream can progress to sepsis and septic shock, which can be life-threatening and require urgent medical intervention.
Ischemia and Necrosis: Severe swelling in the appendix can lead to a reduction in blood supply (ischemia), causing increased inflammation and eventually leading to tissue decay (necrosis).
Abscess: In the initial stages, the infection may not extend far beyond the appendix. It may result in the formation of an abscess, which is a localized pocket of pus on the exterior of the appendix. Additionally, the appendix may develop a mass known as a phlegmon, containing the infection. Both abscesses and phlegmons have the potential to burst, releasing infectious material.
Gangrene/Perforation: Once necrosis sets in, the infection can spread. This may occur gradually through internal gangrene or rapidly if the appendix tears or bursts (perforation). Perforation of the appendix is a critical stage and can lead to the release of infectious material into the abdominal cavity.
The rapid progression of these complications underscores the critical nature of appendicitis. Immediate medical attention is crucial to prevent the condition from advancing to more severe stages and to mitigate the risk of life-threatening complications. Treatment typically involves surgical removal of the inflamed appendix (appendectomy) to prevent further infection and complications. Recognizing the signs and symptoms of appendicitis and seeking prompt medical care are essential for a favorable outcome and to minimize the risk of complications associated with this condition.
Conclusion
In conclusion, grasping the nuances of appendicitis is paramount for safeguarding one's health. This prevalent yet potentially severe condition demands swift recognition and medical intervention to avert complications. Armed with awareness, individuals can proactively prioritize their well-being, potentially sidestepping the grave consequences linked to a ruptured appendix. Recognizing abdominal pain as a serious symptom and seeking immediate medical evaluation can be a life-saving decision. Cura4U emerges as a pivotal ally in proactive health management, extending its comprehensive healthcare services to include early detection and education on conditions like appendicitis. By empowering users to monitor their well-being and detect potential issues, Cura4U fosters a preventive healthcare culture. The platform's commitment to education ensures individuals are well-informed about the risks associated with various conditions, advocating for timely medical intervention. Through a collaborative effort between Cura4U and individuals, we can collectively contribute to a healthier future, underscoring the significance of preventive measures in managing appendicitis and overall well-being.
Our clinical experts continually monitor the health and medical content posted on CURA4U, and we update our blogs and articles when new information becomes available. Last reviewed by Dr. Tayyab Saeed Akhter on December 29th, 2023.
References
Acute appendicitis in young children less than 5 years: review article | Italian Journal of Pediatrics | Full Text (biomedcentral.com) - https://ijponline.biomedcentral.com/articles/10.1186/s13052-017-0335-2
Stages Of Appendicitis: What You Need To Know [2023] (colorectalsurgery.com.sg) - https://colorectalsurgery.com.sg/stages-of-appendicitis/
SciELO - Brazil - PEDIATRIC APPENDICITIS: AGE DOES MAKE A DIFFERENCE PEDIATRIC APPENDICITIS: AGE DOES MAKE A DIFFERENCE - https://www.scielo.br/j/rpp/a/mk9HdYDy69kJkM8gR5p3CNP/
Appendicitis: Practice Essentials, Background, Anatomy (medscape.com) - https://emedicine.medscape.com/article/773895-overview#showall?form=fpf
Appendicitis | Johns Hopkins Medicine - hopkinsmedicine.org/health/conditions-and-diseases/appendicitis#:~:text=Appendicitis happens when the inside,blocked or trapped by stool.
Symptoms & Causes of Appendicitis - NIDDK (nih.gov) - https://www.niddk.nih.gov/health-information/digestive-diseases/appendicitis/symptoms-causes
Appendicitis - StatPearls - NCBI Bookshelf (nih.gov) - https://www.ncbi.nlm.nih.gov/books/NBK493193/
Appendicitis: MedlinePlus Medical Encyclopedia - https://medlineplus.gov/ency/article/000256.htm
Appendicitis - Gastrointestinal Disorders - MSD Manual Professional Edition (msdmanuals.com) - https://www.msdmanuals.com/professional/gastrointestinal-disorders/acute-abdomen-and-surgical-gastroenterology/appendicitis