If your feet feel itchy or sore or you see redness, rashes, or scaling on your soles, you could be experiencing a common skin infection called athlete's foot, also known as tinea pedis. An athlete’s foot is caused by a fungus that thrives in warm and moist environments, and it's prevalent among people who participate in sports and other physical activities that cause sweating and friction on the feet. Similar fungal infections can also affect other body areas, such as jock itch in the groin area and ringworm on various body parts.
In this blog post, we'll provide a comprehensive overview of athlete's foot, its causes, symptoms, diagnosis, and treatment options available for managing the condition. We'll also explore preventive measures to reduce your risk of getting an athlete's foot and how to seek medical attention if needed. Whether you're an athlete or someone simply trying to take better care of your feet, this guide will help you understand athlete's foot and how you can prevent and manage the condition.
Causes and Risk Factors of Athlete's Foot
Athletes’ foot is caused by a fungus called Trichophyton, which thrives in warm and humid environments like public showers, locker rooms, and swimming pools. The infection spreads by contact with infected skin or surfaces, such as towels, socks, or shoes. People who wear tight-fitting or poorly ventilated shoes, those who perspire excessively, and those with weakened immune systems are at a higher risk of getting athlete's foot.
Athletes’ foot is highly contagious and can be easily transmitted through direct contact with infected individuals or contaminated surfaces. Avoid sharing personal items, such as towels, socks, and shoes, to minimize the risk of transmission.
Certain occupations or activities that involve prolonged exposure to damp environments, such as agricultural work or swimming, can increase the risk of developing athlete's foot.
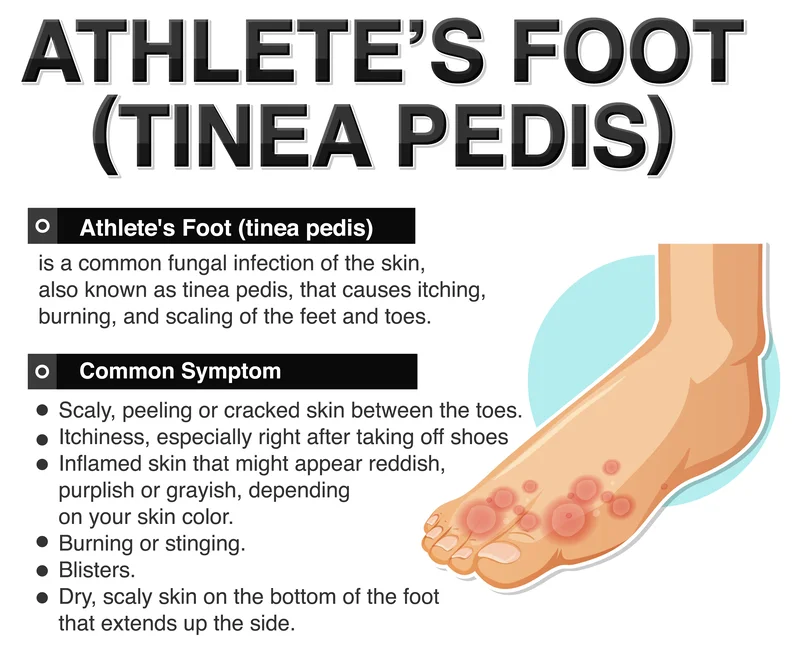
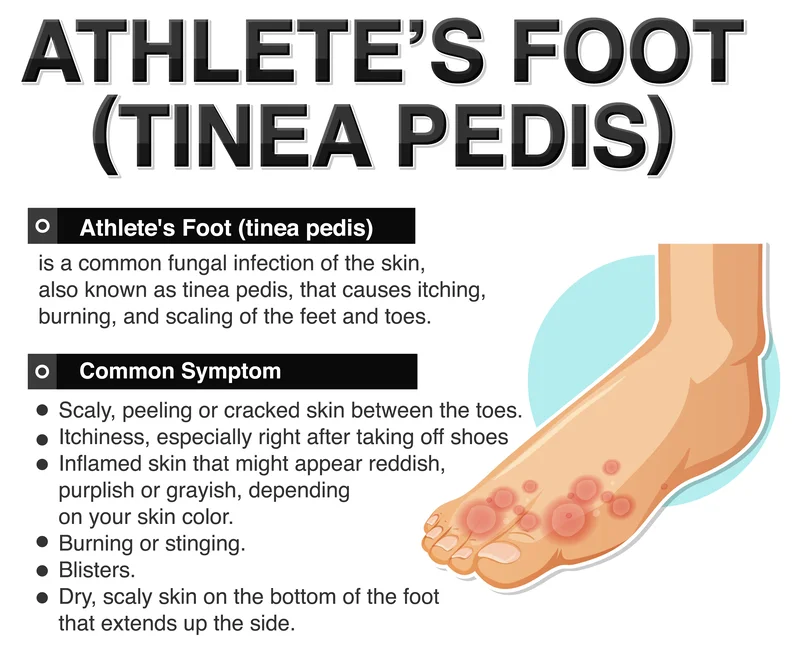
Recognizing the Symptoms of Athlete's Foot
The most common symptoms of athlete's foot include itching, redness, burning, and cracking of the skin between the toes or on the soles of the feet. In severe cases, blisters, ulcers, and foul-smelling discharge may develop. Athlete's foot can also affect the sides and bottoms of the feet and the toenails, leading to toenail discoloration, thickening, and brittleness.
The itching and burning sensation experienced with athlete's foot can intensify during nighttime or after prolonged periods of wearing shoes and socks.
Diagnosis and Evaluation
If you suspect you have athlete's foot, a healthcare professional can diagnose the condition by examining your feet and taking skin scrapings or cultures to identify the fungus. Sometimes, other skin infections or conditions can mimic athlete's foot, so it's crucial to receive a proper evaluation to avoid a mistaken diagnosis. Additional diagnostic techniques that healthcare professionals may employ include using a Wood's lamp (ultraviolet light) to detect certain fungal infections or sending samples for laboratory testing to determine the specific species of fungus involved.
It's important to differentiate between athlete's foot and other conditions, such as eczema or psoriasis, which may require different treatment approaches.
Treatment Options for Athlete's Foot
Several treatment options are available to manage athlete's foot, including over-the-counter antifungal creams, sprays, and powders. These medications work by killing the fungus and preventing it from spreading. Sometimes, oral antifungal medications may be necessary to treat more severe or persistent infections.
Completing the full course of treatment is crucial when managing athlete's foot effectively. Even if your symptoms start to improve or disappear, it's important to continue using the prescribed antifungal medications for the recommended duration. This is because fungal infections can be stubborn and linger even after symptoms have resolved. Adhering to the entire treatment course ensures that the fungus is completely eradicated, reducing the risk of recurrence.
In addition to medication, healthcare professionals may suggest using antifungal foot powders or sprays as part of your athlete's foot management plan. These products are designed to help keep your feet dry and create an environment that is less favorable for fungal growth. The antifungal properties of these powders or sprays can further prevent the recurrence of athlete's foot. Incorporating them into your daily foot care routine, especially when participating in physical activities or environments prone to moisture, provides extra protection against the fungus and promotes faster healing.
Remember to follow your healthcare professional's recommendations regarding the specific products, the application method, and the frequency of use. These measures, combined with proper foot hygiene and other preventive strategies, can help you effectively manage athlete's foot and reduce the risk of future infections. Additionally, maintaining good foot hygiene, wearing loose-fitting shoes made of breathable materials, and drying your feet thoroughly after showering can prevent the recurrence of athlete's foot.
Preventive Measures to Avoid Athlete's Foot
Several practical tips can help reduce your risk of getting athlete's foot:
- Avoid walking barefoot in public areas, such as communal showers, locker rooms, and pool decks.
- Change socks and shoes frequently, especially if damp or sweaty.
- Wash your feet regularly with soap and warm water, ensuring thorough drying, particularly between the toes.
- Choose socks made of moisture-wicking materials, such as cotton or wool blends, to help keep the feet dry and minimize the risk of fungal growth.
- Use antifungal powders or sprays in shoes, especially during physical activities or environments prone to moisture accumulation.
- Avoid sharing personal items like towels, socks, and shoes with others, as this can increase the spread of the fungus.
When to Seek Medical Attention
If you experience severe or persistent symptoms of athlete's foot, such as the development of open sores or the spread of infection to other parts of the body, seek medical attention promptly. Additionally, people with diabetes, peripheral artery disease, and other conditions that affect their feet should be checked regularly by a healthcare professional.
Specific examples of severe symptoms or complications that warrant immediate medical attention are:
- Presence of fever: If you have athlete's foot and develop a fever, it may indicate a more serious infection or secondary complications. Fever is generally not associated with athlete's foot alone, so it's important to seek medical attention promptly.
- Increasing pain: If you notice that the pain associated with your athlete's foot intensifies over time, it could be a sign of a more severe infection or the involvement of deeper tissues. Consulting a healthcare professional is essential in such cases.
- Rapid spreading of the infection: Athlete's foot typically starts between the toes but can quickly spread to other areas of the foot or even to other parts of the body. If you notice that the infection is rapidly spreading, it may require immediate medical attention to prevent further complications.
- Signs of cellulitis (such as redness, warmth, and swelling extending beyond the foot): Cellulitis is a bacterial skin infection that can occur as a complication of athlete's foot. If you observe redness, warmth, swelling, and spreading of these symptoms beyond the foot, it could indicate cellulitis. Cellulitis requires prompt medical evaluation and treatment.
Individuals with compromised immune systems should promptly consult with their healthcare providers if they suspect they have athlete's foot:
- People with HIV/AIDS: Those who have HIV/AIDS often have weakened immune systems, which can make them more susceptible to infections, including athlete's foot. If individuals with HIV/AIDS suspect they have athlete's foot, they should consult their healthcare providers promptly to prevent the infection from worsening or spreading.
- Individuals undergoing chemotherapy: Chemotherapy weakens the immune system as part of cancer treatment. Consequently, individuals undergoing chemotherapy should be cautious about any signs of athlete's foot and seek immediate medical advice if they suspect an infection. Prompt intervention can help prevent potential complications and ensure appropriate management.
Remember, it's always important to consult a healthcare professional for personalized advice and appropriate treatment options, especially when dealing with severe symptoms or when your immune system is compromised.
Complications and Long-Term Management of Athlete’s Foot
In some cases, untreated or poorly managed athlete's foot can lead to secondary bacterial infections, cellulitis, or the fungus spread to other parts of the body, such as the nails or groin. Long-term management of athlete's foot involves adopting good foot hygiene practices, preventing reinfection, and promptly treating any symptoms that arise.
Fungal Infections Related to Athlete's Foot: Jock Itch and Ringworm
In addition to athlete's foot (tinea pedis), two other common fungal infections share similar characteristics and causes. These are jock itch (tinea cruris) and ringworm (tinea corporis). Like athlete's foot, both jock itch and ringworm are caused by fungi and thrive in warm and moist environments.
Jock itch primarily affects the groin area, inner thighs, and buttocks, often causing redness, itching, and a rash that may have a distinct border. It is commonly seen in athletes, particularly those who engage in activities that cause excessive sweating, friction, and wearing tight-fitting clothing.
On the other hand, ringworm can occur on various body parts and is characterized by circular or ring-shaped rashes that are itchy, red, and scaly. It can affect the scalp (tinea capitis), body (tinea corporis), or even the nails (tinea unguium). Ringworm can be transmitted through direct contact with infected humans or animals and contaminated objects or surfaces.
All three conditions, athlete's foot, jock itch, and ringworm, are caused by dermatophytes, a group of fungi that feed on keratin, a protein found in the skin, hair, and nails. They share common risk factors such as warm and moist environments, compromised skin integrity, excessive sweating, and poor hygiene practices. Although each infection may have distinct symptoms and affect different body areas, they can often be managed with similar antifungal treatments, including over-the-counter creams, sprays, or oral medications in more severe cases. Maintaining good hygiene, keeping the affected areas clean and dry, and avoiding sharing personal items can help prevent the spread and recurrence of these fungal infections.
If you suspect you have a jock itch, ringworm, or athlete's foot, it's essential to consult a healthcare professional for an accurate diagnosis and appropriate treatment plan. They can provide personalized advice and recommend the most effective antifungal medications to alleviate symptoms and promote healing. Understanding the similarities and differences among these fungal infections can empower you to take proactive steps to care for your skin and prevent future infections.
Conclusion
In conclusion, athlete's foot is a common skin infection that can cause discomfort and affect your quality of life. With proper prevention, early detection, and prompt treatment, you can manage the condition effectively and avoid complications. If you're experiencing symptoms of athlete's foot, talk to your healthcare professional for an evaluation and personalized treatment plan.
At Cura4U, we offer various primary healthcare services, including telemedicine consultations, to help you manage your foot health from the comfort of your home. Book an appointment with our healthcare professionals today to learn more about how we can help you manage athlete's foot and other common conditions.
Our clinical experts continually monitor the health and medical content posted on CURA4U, and we update our blogs and articles when new information becomes available. Last reviewed by Dr. Tayyab Saeed Akhter on June 26th, 2023.
References
Hygiene-related Diseases | Hygiene-related Diseases | Hygiene | Healthy Water | CDC
Tinea Pedis (Athlete's Foot) - Dermatologic Disorders - MSD Manual Professional Edition (msdmanuals.com)- https://www.msdmanuals.com/professional/dermatologic-disorders/fungal-skin-infections/tinea-pedis-athlete-s-foot
Athlete's foot: Overview - InformedHealth.org - NCBI Bookshelf (nih.gov)- https://www.ncbi.nlm.nih.gov/books/NBK279549/
Athlete's Foot | Tinea Pedis | MedlinePlus- https://medlineplus.gov/athletesfoot.html
Tinea Pedis - StatPearls - NCBI Bookshelf (nih.gov)- https://www.ncbi.nlm.nih.gov/books/NBK470421/#:~:text=Tinea%20pedis%20or%20foot%20ringworm,Africa%2C%20Asia%2C%20and%20Australia.
Tinea Pedis: Background, Pathophysiology, Epidemiology (medscape.com)- https://emedicine.medscape.com/article/1091684-overview