Osteoporosis is a common condition that weakens bones and increases the risk of fractures, particularly among older adults. Despite its prevalence, many people are unaware of effective strategies for managing osteoporosis. This comprehensive blog post will explore various strategies, including medication, nutrition, exercise, lifestyle modifications, and managing coexisting conditions. Whether you are a patient, family member, or caregiver, this information is important for improving bone health and overall well-being.
Understanding Osteoporosis
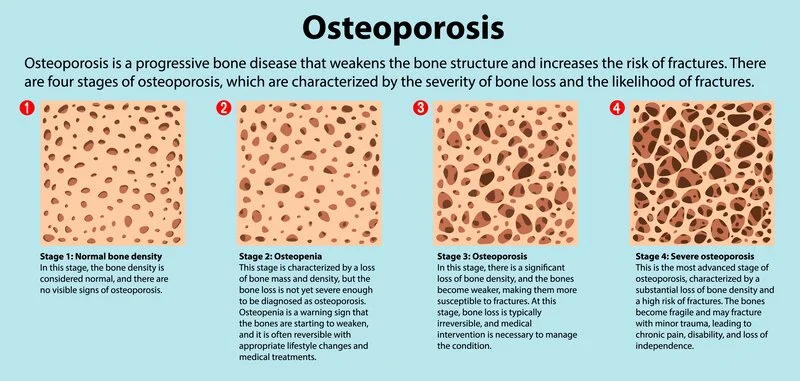
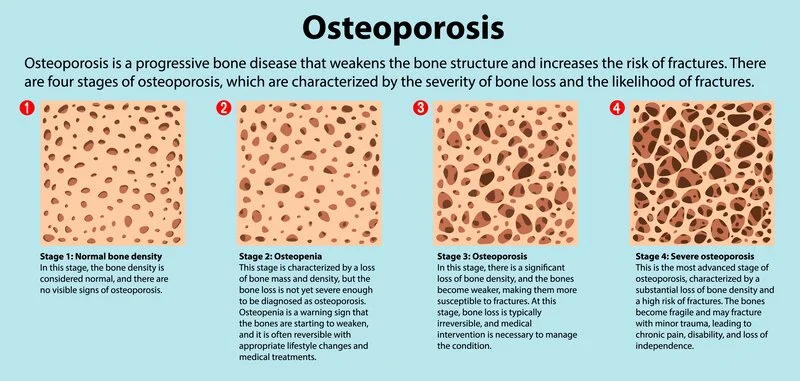
Osteoporosis is a complex condition characterized by reduced bone density, leading to weakened bones that are highly susceptible to fractures. While bone density naturally decreases with age, osteoporosis accelerates this process, significantly impacting an individual's quality of life. It is alarming to note that over 200 million people worldwide are affected by osteoporosis, making it a widespread health concern. Furthermore, studies estimate that osteoporosis causes more than 8.9 million fractures annually, highlighting this condition's seriousness and substantial impact on individuals and healthcare systems globally. Understanding the prevalence and gravity of osteoporosis is essential for promoting awareness and implementing effective preventive measures and treatment strategies.
Understanding Bone Health
Bones are remarkable living tissues that undergo constant remodeling throughout our lives. This dynamic process involves a delicate balance between the breakdown of old bone tissue (resorption) and the formation of new bone tissue (formation). This balance helps maintain the strength, structure, and density of our bones. However, in individuals with osteoporosis, this equilibrium is disrupted, leading to a significant increase in bone resorption compared to bone formation. Over time, this gradual loss of bone density compromises bone strength and resilience, resulting in weakened bones that are highly vulnerable to fractures. Understanding the underlying mechanisms of bone remodeling and how osteoporosis disrupts this process is crucial for developing targeted interventions and management strategies to prevent bone loss and minimize fracture risk.
Risk Factors for Osteoporosis
Various factors contribute to an individual's risk of developing osteoporosis. These risk factors include age, genetics, hormonal changes, inadequate calcium or vitamin D intake, certain medications, smoking, excessive alcohol consumption, and a sedentary lifestyle. Advancing age is a significant risk factor, as bone density naturally declines as we age, making older adults more susceptible to osteoporosis. Women over the age of 50, in particular, face a higher risk, with statistics showing that one in three women will experience an osteoporotic fracture in their lifetime. Genetic factors also play a role, as individuals with a family history of osteoporosis are more likely to develop the condition. Hormonal changes, such as those that occur during menopause, can accelerate bone loss in women. Additionally, lifestyle factors such as low calcium or vitamin D intake, smoking, excessive alcohol consumption, and a sedentary lifestyle contribute to increased osteoporosis risk. Recognizing these risk factors and taking appropriate preventive measures, including lifestyle modifications and regular screenings, is crucial for reducing the likelihood of developing osteoporosis and preventing fractures.

Diagnosis and Assessment
Accurate diagnosis and ongoing assessment are crucial for effectively managing osteoporosis. A comprehensive evaluation of your bone health helps determine your risk of developing the condition or assess the presence of osteoporosis. The most commonly used diagnostic test is a bone density scan, also known as dual-energy X-ray absorptiometry (DXA). This painless and non-invasive procedure measures the density of your bones in key areas, such as the hip and spine, providing valuable information about their strength and integrity. Low radiation levels create detailed images of your bones during a bone density scan. These images are then analyzed to calculate your bone mineral density (BMD) and compare it to the expected values for someone of your age and sex. Based on the results, your healthcare provider can determine if you have osteoporosis, identify the severity of the condition, or evaluate your risk of developing it in the future. In addition to bone density scans, your healthcare provider may consider other factors in the diagnosis and assessment of osteoporosis. These include evaluating your medical history, assessing your risk factors, performing physical examinations, and ordering blood tests to measure specific markers of bone turnover and hormone levels. A comprehensive evaluation ensures a thorough understanding of your bone health status and aids in developing a personalized treatment plan.
Regular bone health check-ups and monitoring are essential for assessing changes in your bone density over time. These check-ups allow your healthcare provider to track the effectiveness of your current treatment plan, make necessary adjustments, and provide early intervention if needed. Monitoring your bone health status enables proactive management and reduces the risk of fractures.
It's important to remember that qualified healthcare professionals should always diagnose and assess osteoporosis. They have the expertise and access to the necessary diagnostic tools to accurately evaluate your bone health and provide appropriate recommendations for treatment and management. Regular follow-ups and open communication with your healthcare provider are key to maintaining optimal by and overall well-being.

Medications for Osteoporosis
Several medications are available to manage osteoporosis effectively. Bisphosphonates, such as alendronate and risedronate, are commonly prescribed. They work by slowing down bone remodeling, reducing the loss of bone density, and decreasing the risk of fractures. Hormone-related therapy (HRT) is another option, particularly for postmenopausal women. Additionally, newer medications such as denosumab and selective estrogen receptor modulators (SERMs) have shown efficacy in preventing bone loss and fractures. It is important to consult with your doctor to understand the different medication options available and determine the most suitable one for you. It's crucial to mention potential side effects or considerations associated with each medication, such as gastrointestinal discomfort, jaw problems, or the need for regular dental check-ups with bisphosphonates.
Nutrition for Bone Health
Maintaining proper nutrition is vital for bone health and preventing osteoporosis. Calcium and vitamin D are critical nutrients for strong bones. Calcium-rich foods such as dairy products (milk, cheese, yogurt), leafy greens (kale, spinach, and broccoli), and fortified foods (cereals and juices) should be incorporated into the diet. Did you know adults over 50 require 1,200 to 1,500 milligrams of calcium daily? Vitamin D can be obtained through sunlight exposure or supplements. Additionally, it's important to mention the role of other micronutrients, such as vitamin K, magnesium, and phosphorus, in supporting bone health. A balanced diet that includes fruits, vegetables, whole grains, and lean proteins provides essential nutrients for overall health and well-being. Consulting with a doctor or registered dietitian ensures you are receiving adequate nutrition for bone health.
Exercise and Physical Activity
Engaging in regular physical activity and exercise is beneficial for maintaining bone density and preventing further bone loss. Weight-bearing exercises, including running, dancing, jumping rope, and weightlifting, are particularly effective in improving bone health. These activities place stress on the bones, stimulating them to become stronger. Strength training exercises also help build muscle, which supports bone health. Additionally, incorporating balance and coordination exercises like yoga or tai chi can reduce the risk of falls and fractures. Remember to consult your doctor or a physical therapist to determine the exercise types best suited for your situation, including fall prevention exercises and home safety recommendations.
Non-Pharmacological Approaches to Managing Osteoporosis
Non-pharmacological approaches play a significant role in managing osteoporosis. Fall prevention exercises, such as balance training and proprioceptive exercises, help improve stability and reduce the risk of falls. These exercises can be performed under the guidance of a physical therapist or as part of a specialized program. Focusing on exercises that improve coordination, strength, and flexibility is important. Implementing various lifestyle modifications can positively impact bone health. Quitting smoking is crucial, as studies have shown that smoking increases bone loss and fracture risk. Maintaining a healthy weight is important, too; excessive weight strains the bones, while being underweight increases the risk of bone loss. Limiting alcohol intake is recommended, as excessive consumption decreases bone formation and increases fracture risk. Additionally, making necessary modifications to your home environment, such as removing tripping hazards, improving lighting, and using assistive devices such as grab bars in bathrooms, can significantly reduce the risk of falls and fractures. Furthermore, avoiding certain medications, such as corticosteroids, is crucial as they can increase the risk of osteoporosis. It is important to consult your healthcare provider to discuss valuable recommendations that can help improve your bone health and overall well-being.
Managing Coexisting Conditions
In addition to addressing osteoporosis, it is important to recognize and manage any coexisting medical conditions that may increase the risk or exacerbate the progression of osteoporosis. Certain conditions, such as inflammatory bowel disease, celiac disease, or chronic kidney disease, are more associated with osteoporosis.
A multifaceted approach is often necessary to effectively manage coexisting conditions and minimize their impact on bone health. This may involve appropriate medical treatment tailored to the specific condition, such as medications to control inflammation in inflammatory bowel disease or adherence to a strict gluten-free diet in celiac disease. The risk of developing osteoporosis or the progression of existing osteoporosis can be reduced by effectively managing these underlying conditions. It is crucial to have open and proactive communication with your healthcare provider to discuss strategies for managing coexisting conditions and their potential impact on bone health. Working collaboratively with your healthcare team ensures comprehensive care and optimizes your overall health and well-being, including managing osteoporosis and coexisting conditions.

The Future of Osteoporosis Management
Research in the field of osteoporosis management is continuously uncovering new insights and advancements that hold promise for improved outcomes. Several notable research areas and advancements in osteoporosis management include:
· Bone-Targeted Therapies: Researchers are exploring innovative medications targeting bone-regulating mechanisms to enhance bone formation and reduce bone resorption by considering care options like Respite Care can assist caregivers in providing breaks.. For example, studies are investigating the effectiveness of monoclonal antibodies that inhibit specific proteins involved in bone breakdown, such as sclerostin. These medications have shown potential in increasing bone density and reducing fracture risk.
· Combination Therapies: Researchers are studying the potential benefits of combining different classes of medications to optimize treatment outcomes. For instance, clinical trials evaluate the efficacy and safety of combining antiresorptive medications (e.g., bisphosphonates) with anabolic agents (e.g., teriparatide) to achieve synergistic effects on bone health.
· Advances in Imaging Techniques: Imaging technologies, such as high-resolution peripheral quantitative computed tomography (HR-pQCT), are refined to provide more detailed information about bone structure and quality. These advancements enable better assessment of bone health and help predict fracture risk with greater accuracy.
· Personalized Medicine: Personalized medicine is gaining traction in osteoporosis management. Genetic testing and identifying specific genetic markers associated with osteoporosis susceptibility may help tailor treatment plans to individual patients, improving treatment effectiveness and reducing adverse effects.
· Nutritional Approaches: Researchers are investigating the role of various nutrients and dietary factors in bone health. For example, studies are exploring the potential benefits of specific dietary patterns, such as the Mediterranean diet, in promoting bone health and reducing the risk of fractures.
· Exercise Interventions: Ongoing research focuses on optimizing exercise interventions for individuals with osteoporosis. Studies examine the effects of different exercise modalities, such as high-intensity resistance training, weight-bearing activities, and balance and coordination exercises, on bone density, strength, and fracture prevention.
It is important to note that while these advancements show promise, further research and clinical trials are necessary to establish their long-term effectiveness, safety, and applicability to different populations. Staying informed about ongoing research and discussing potential advancements with healthcare professionals can help individuals make informed decisions about their osteoporosis management and benefit from emerging therapies in the future.
Conclusion
Managing osteoporosis requires a comprehensive approach encompassing medication, nutrition, exercise, and lifestyle modifications. Working closely with your healthcare provider and following a personalized plan can help improve bone health and overall well-being. Remember to consult with healthcare professionals for proper osteoporosis evaluation, diagnosis, and management. Educating yourself about the warning signs, risk factors, and available strategies for managing osteoporosis is the first step toward taking control of your bone health. With these strategies in place, a diagnosis of osteoporosis doesn't have to limit your quality of life.
Cura4U is a comprehensive healthcare platform designed to meet all your osteoporosis-related medical requirements. Our primary goal is to offer convenient access to various healthcare services. You can effortlessly schedule appointments with doctors specializing in osteoporosis and access lab tests and radiology services from the comfort of your own home. You can trust Cura4U to provide the necessary care to maintain your health and well-being, ensuring that you receive the appropriate services at affordable prices. Stay proactive, stay informed, and prioritize your bone health for a stronger future.
Our clinical experts continually monitor the health and medical content posted on CURA4U, and we update our blogs and articles when new information becomes available. Last reviewed by Dr. Tayyab Saeed Akhter on June 27th, 2023.
References
Osteoporosis Causes & Symptoms | NIAMS (nih.gov)
Osteoporosis | National Institute on Aging (nih.gov)
Osteoporosis - NHS (www.nhs.uk)- https://www.nhs.uk/conditions/osteoporosis/
Osteoporosis: Practice Essentials, Background, Pathophysiology (medscape.com)- https://emedicine.medscape.com/article/330598-overview
HR-pQCT Measures of Bone Microarchitecture Predict Fracture: Systematic Review and Meta-Analysis - PubMed (nih.gov)- https://pubmed.ncbi.nlm.nih.gov/31643098/
Osteoporosis - OrthoInfo - AAOS- https://orthoinfo.aaos.org/en/diseases--conditions/osteoporosis/
Osteoporosis (rheumatology.org)- https://rheumatology.org/patients/osteoporosis
Does Osteoporosis Run in Your Family? | CDC
An overview and management of osteoporosis - PMC (nih.gov)- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5335887/
A comprehensive overview on osteoporosis and its risk factors | TCRM (dovepress.com)- https://www.dovepress.com/a-comprehensive-overview-on-osteoporosis-and-its-risk-factors-peer-reviewed-fulltext-article-TCRM
The global prevalence of osteoporosis in the world: a comprehensive systematic review and meta-analysis | Journal of Orthopaedic Surgery and Research | Full Text (biomedcentral.com)- https://josr-online.biomedcentral.com/articles/10.1186/s13018-021-02772-0
The pathogenesis, diagnosis, investigation and management of osteoporosis | Journal of Clinical Pathology (bmj.com)- https://jcp.bmj.com/content/64/12/1042
Bone-Targeted Therapy - PMC (nih.gov)- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4490911/
Combination therapy for osteoporosis: a reappraisal - PMC (nih.gov)- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4007166/