Vitamin D is a crucial nutrient that plays a significant role in the human body. It contributes to many important functions, including calcium absorption, bone health, immune support, hormonal regulation, mental well-being, and disease prevention. Therefore, understanding and optimizing Vitamin D levels is essential. In this comprehensive guide, we will explore the fundamentals of Vitamin D, its various forms, and the critical functions and benefits that it provides. We will also discuss sources and supplementation of Vitamin D, understanding Vitamin D levels and deficiency, common risk factors, signs and symptoms, and the potential health implications. Finally, we will provide practical recommendations to optimize Vitamin D levels, including lifestyle and dietary strategies and the importance of monitoring and supplementing under healthcare professional guidance.
Overview of Vitamin D
Vitamin D is an essential fat-soluble vitamin crucial in various physiological processes within the human body. While sunlight is the primary source of vitamin D, it can also be obtained from certain foods and supplements. When the skin is exposed to ultraviolet B (UVB) radiation from sunlight, a precursor molecule called 7-dehydrocholesterol, present in the skin, undergoes a complex conversion process, ultimately forming vitamin D3 (cholecalciferol). However, the production of vitamin D3 is influenced by several factors. Individuals with darker skin pigmentation have higher levels of melanin, which can reduce the skin's ability to produce vitamin D3. Consequently, darker skin requires more sun exposure than lighter skin to generate adequate amounts of vitamin D3. However, optimal sun exposure practices need to be balanced with the need for sun protection to prevent skin damage. Other factors that affect vitamin D production include latitude (higher latitudes receive less intense sunlight), time of day (midday sun is most effective for vitamin D synthesis), and season (less sunlight during winter months). Spending 15-20 minutes in the sun daily, during the early morning or late afternoon, without sunscreen, is recommended to facilitate vitamin D synthesis.
It is important to consider personal factors such as skin type, geographic location, time of day, and season when determining the appropriate strategies for obtaining adequate vitamin D while maintaining skin health.
Vitamin D and Its Various Forms (D2 and D3)
Vitamin D has two main forms: Vitamin D2 (ergocalciferol) and Vitamin D3 (cholecalciferol). These forms differ in their origin and potency. Vitamin D2 is synthesized by plants when exposed to ultraviolet (UV) light. On the other hand, Vitamin D3 is produced in the skin of humans and animals when exposed to UV light. This synthesis occurs from a cholesterol derivative present in the skin. It is worth noting that Vitamin D3 is considered to be more biologically active and potent than Vitamin D2. Consequently, Vitamin D3 is the preferred form for supplementation and is often more effective at raising and maintaining optimal vitamin D levels in the body. When considering vitamin D supplementation, it is advisable to choose Vitamin D3 to maximize its benefits.
Sources of Vitamin D
Vitamin D can be obtained from various sources, with sunlight being the primary and most natural source. Safe and sensible sun exposure is crucial for stimulating vitamin D synthesis in the skin. However, it's important to note that excessive sunlight exposure without proper protection can increase the risk of skin damage. It is recommended to balance sun exposure for vitamin D synthesis with the need for sun protection. Remember, excessive exposure to UV radiation can increase the risk of sunburn, premature skin aging, and skin cancer. It's crucial to balance obtaining sufficient vitamin D and protecting your skin from harmful UV rays. If you have concerns about sun exposure or skin health, consult a healthcare professional or dermatologist for personalized advice.
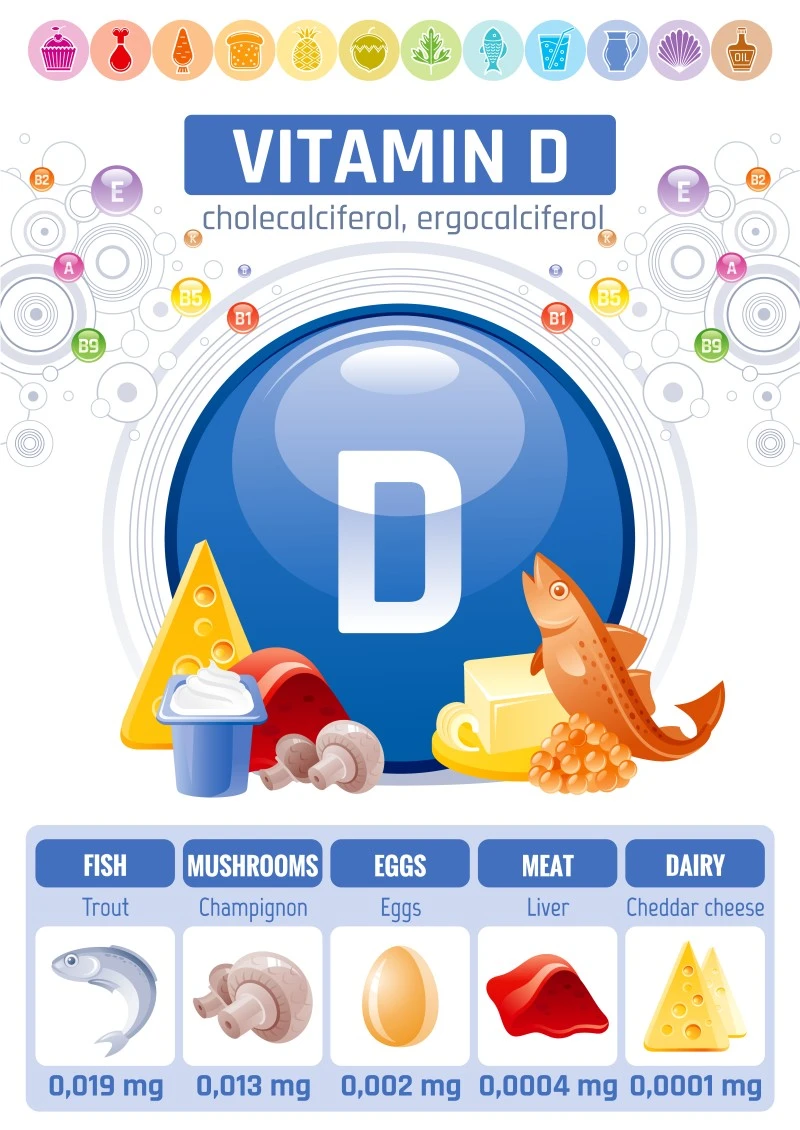
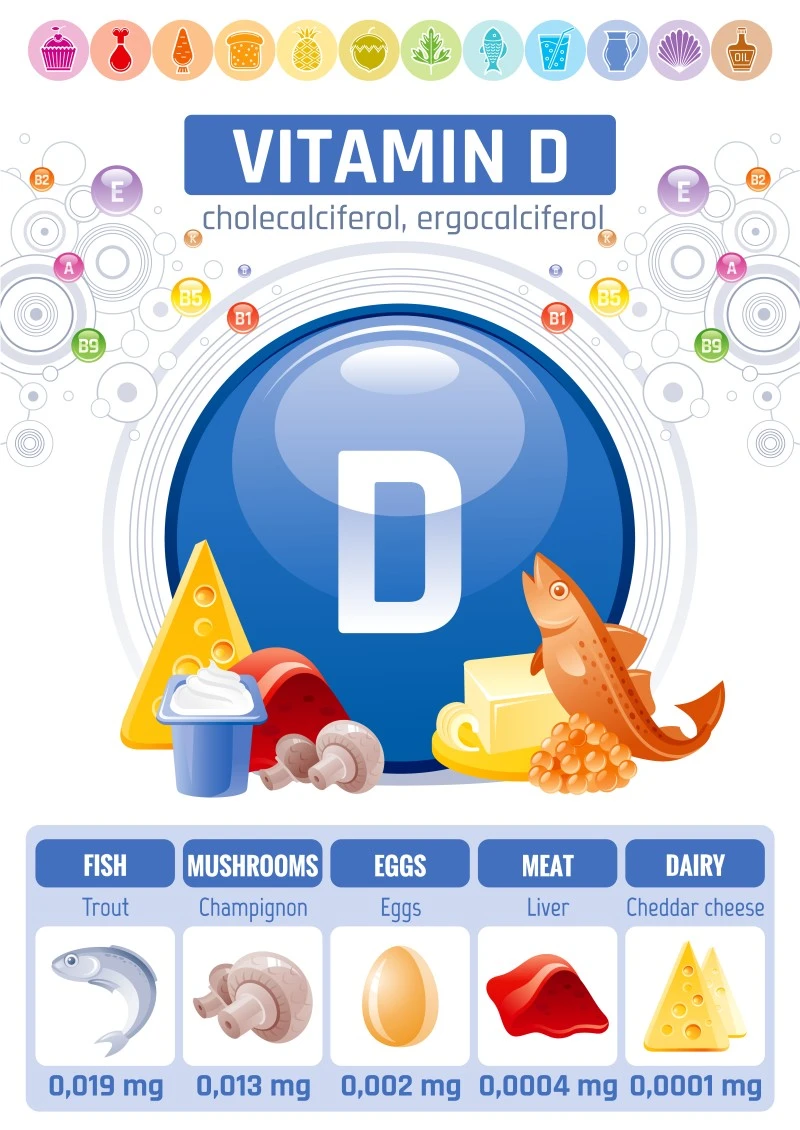
In addition to sunlight, certain foods also contain Vitamin D. Oily fish, such as salmon, sardines, and mackerel, are excellent sources of Vitamin D. These fish accumulate Vitamin D3 in their fatty tissues through their diet or sun exposure. Egg yolks also contain small amounts of Vitamin D. Furthermore, fortified foods play a significant role in providing Vitamin D. Milk, cereal, and orange juice are commonly fortified with Vitamin D to help individuals meet their daily requirements. By combining sunlight exposure and consuming foods rich in Vitamin D, individuals can ensure an adequate intake of this essential nutrient. However, it's important to note that for those with limited sun exposure, specific medical conditions, or other factors that increase the risk of deficiency, supplementation may be necessary under the guidance of a healthcare professional.
Functions and Benefits of Vitamin D
Vitamin D plays a critical role in several key functions within the body. One of its primary functions is facilitating the absorption of calcium, which is essential for maintaining strong and healthy bones. In addition to bone health, vitamin D also supports the immune system, helps regulate hormones, promotes mental well-being, and aids in disease prevention.
Research studies have explored the association between vitamin D deficiency and various health conditions. Findings suggest inadequate vitamin D levels may be linked to an increased risk of autoimmune diseases, cardiovascular disorders, mental health conditions, and certain cancers. However, it is important to note that vitamin D deficiency does not directly cause these conditions. Instead, it may contribute to an elevated risk or act as a contributing factor. While the relationship between vitamin D and these health conditions is complex and requires further investigation, it is advisable to consult with your doctor if you suspect you might have a vitamin D deficiency and if it could be a factor in developing these conditions. Your doctor can provide appropriate evaluation, guidance, and recommendations based on your circumstances.
Role of Vitamin D in Calcium Absorption
Vitamin D promotes calcium absorption in the intestines, ensuring that an adequate amount of calcium is absorbed from the diet and into the bloodstream. It does this by enhancing the expression of calcium transport proteins in the intestinal cells, increasing the efficiency of calcium absorption. This is crucial for maintaining bone health, as calcium is essential for skeletal development and maintaining strong and healthy bones. Calcium is also necessary for muscle function, allowing muscles to contract and relax properly. Furthermore, calcium is involved in nerve signaling, playing a role in transmitting signals between nerve cells.
Mechanisms of Vitamin D in Immune Support
Vitamin D supports the immune system through various mechanisms. Firstly, it influences immune cell function by regulating the production and activity of immune cells, such as T cells, B cells, and macrophages. Vitamin D helps maintain a balanced immune response, preventing excessive inflammation while promoting an effective immune defense against pathogens. Secondly, it modulates inflammatory responses by reducing the production of pro-inflammatory cytokines and increasing the production of anti-inflammatory cytokines. This helps regulate the immune system's response to inflammation. Lastly, recent research suggests that vitamin D may have direct antiviral effects, potentially inhibiting the replication of certain viruses within the body.
Relationship Between Vitamin D and Mental Well-being
Vitamin D has been linked to mental health and well-being. It is thought to play a role in regulating mood and reducing the risk of depression. Vitamin D receptors are present in brain areas involved in mood regulation. Low vitamin D levels have been associated with an increased risk of depression and other mood disorders. Additionally, vitamin D may positively impact cognitive function, including memory and executive function. However, more research is needed to fully understand the mechanisms underlying the relationship between vitamin D and mental well-being.
Vitamin D Deficiency and Autoimmune Diseases
Vitamin D deficiency has been linked to autoimmune diseases, which occur when the immune system mistakenly attacks the body's tissues. Vitamin D plays a role in modulating immune responses, helping to maintain immune tolerance and prevent excessive immune activation. Deficiency in vitamin D may contribute to dysregulated immune responses and an increased risk of autoimmune conditions. Specific autoimmune diseases associated with vitamin D deficiency include multiple sclerosis, rheumatoid arthritis, and systemic lupus erythematosus (SLE). While the exact mechanisms are not fully understood, research suggests that vitamin D's immunomodulatory effects play a crucial role in developing and progressing these autoimmune diseases.
Relationship Between Vitamin D and Cardiovascular Health
Vitamin D also plays a role in cardiovascular health. Research has indicated that vitamin D deficiency is associated with an increased risk of cardiovascular diseases, including hypertension, heart disease, and stroke. Vitamin D may help regulate blood pressure by influencing the renin-angiotensin-aldosterone system, which regulates blood pressure. It may also improve endothelial function, which is essential for maintaining the health and flexibility of blood vessels. Additionally, vitamin D has anti-inflammatory properties, and chronic inflammation is a risk factor for cardiovascular disease.
Understanding Vitamin D Levels and Deficiency
Assessing and understanding one's Vitamin D levels is essential for optimizing health. Vitamin D levels can be measured through a common blood test called the 25-hydroxyvitamin D [25(OH)D] test. This test provides valuable information about vitamin D concentration in the blood. Regular testing allows you to monitor your vitamin D levels and make necessary adjustments to your dietary, lifestyle, or supplementation approaches to maintain optimal levels. The optimal range for Vitamin D levels can vary based on factors such as age and specific health conditions. However, a generally desirable range falls between 30-50 ng/mL (nanograms per milliliter). This range is associated with sufficient Vitamin D status and supports the various functions and benefits provided by this essential nutrient.
Levels below 20 ng/mL indicate Vitamin D deficiency. When Vitamin D levels fall below this threshold, individuals may be at a higher risk of experiencing the detrimental effects of deficiency, such as impaired calcium absorption, compromised bone health, weakened immune function, and increased susceptibility to certain diseases.
It is important to note that while a range of 30-50 ng/mL is generally considered desirable, specific recommendations may vary depending on individual circumstances. Healthcare professionals can provide personalized guidance and interpret the test results in the context of an individual's overall health and specific needs.
Regular monitoring of Vitamin D levels is recommended to ensure that levels remain within the optimal range. This monitoring helps individuals track their progress and adjust to lifestyle, diet, and supplementation to maintain adequate Vitamin D levels. Consulting with a healthcare professional is crucial to obtain accurate and reliable test results and to receive appropriate guidance on addressing Vitamin D deficiency, if present.
Common Causes and Risk Factors of Vitamin D Deficiency
Vitamin D deficiency can arise due to various causes and risk factors contributing to inadequate levels of this essential nutrient in the body. Recognizing these common causes and risk factors is crucial for understanding the prevalence and susceptibility to Vitamin D deficiency.
· Inadequate Sun Exposure: Insufficient exposure to sunlight, especially in individuals who spend limited time outdoors or frequently use sunscreen with high sun protection factor (SPF), can hinder the body's ability to produce Vitamin D naturally.
· Limited Dietary Intake: A diet lacking in Vitamin D-rich foods, such as fatty fish (salmon, sardines, mackerel), fortified dairy products, egg yolks, and mushrooms, can contribute to Vitamin D deficiency.
· Darker Skin Pigmentation: Individuals with darker skin pigmentation have higher levels of melanin, which reduces the skin's ability to produce Vitamin D upon exposure to sunlight. Consequently, they may require more extended sun exposure to synthesize adequate levels of Vitamin D.
· Geographical Location: People living in higher latitudes, where sunlight is less intense, may experience reduced Vitamin D synthesis in the skin, especially during winter when daylight hours are shorter.
· Aging: With advancing age, the skin's ability to produce Vitamin D declines, making older individuals more prone to deficiency.
· Obesity: Vitamin D is fat-soluble, and excess adipose tissue can sequester Vitamin D, reducing its bioavailability and contributing to lower circulating levels.
· Medical Conditions: Certain medical conditions, such as celiac disease, Crohn's disease, and kidney disorders, can impair the absorption, metabolism, or activation of Vitamin D in the body.
· Medications: Some medications, including glucocorticoids (steroids), anticonvulsants, and certain cholesterol-lowering drugs, may interfere with Vitamin D metabolism or absorption, leading to deficiency.
· Limited Sunlight Exposure Due to Lifestyle or Occupation: Certain occupations or lifestyle factors that involve indoor work or limited outdoor activities can reduce sun exposure and hinder Vitamin D synthesis.
· Malabsorption Disorders: Conditions that affect the gastrointestinal tract, such as inflammatory bowel disease or surgical removal of parts of the intestine, can impair the absorption of dietary Vitamin D.
Recognizing these common causes and risk factors can help individuals identify potential factors contributing to Vitamin D deficiency. Regular monitoring of Vitamin D levels and consultation with a healthcare professional can guide appropriate interventions, including lifestyle modifications and targeted supplementation, to optimize Vitamin D status and overall health.
Common Signs and Symptoms Associated with Vitamin D Deficiency
Vitamin D deficiency can manifest through various signs and symptoms, indicating an inadequate level of this vital nutrient in the body. Recognizing these common signs and symptoms can help individuals identify the potential presence of Vitamin D deficiency and seek appropriate intervention.
· Muscle Weakness: Vitamin D plays a role in muscle function and strength. Inadequate Vitamin D levels can lead to muscle weakness, making everyday tasks more challenging and affecting overall physical performance.
· Chronic Fatigue: Vitamin D deficiency has been associated with feelings of persistent fatigue and low energy levels. Individuals may experience a general sense of tiredness and lack of motivation.
· Bone Pain: Vitamin D is crucial for maintaining bone health. Insufficient Vitamin D levels can result in bone pain, often felt as a dull, achy sensation. This can occur in different body parts, such as the back, hips, or legs.
· Rickets (in Children): Severe Vitamin D deficiency in children can lead to a condition called rickets. Rickets causes weak and deformed bones, leading to delayed growth, bowed legs, and other skeletal abnormalities.
· Increased Risk of Fractures and Falls: Inadequate Vitamin D levels can compromise bone health and increase the risk of fractures, particularly in older adults. Vitamin D plays a vital role in maintaining bone density and strength, and deficiency can make bones more susceptible to fractures. Vitamin D deficiency may also contribute to impaired muscle function and balance, increasing the risk of falls.
It is important to note that these signs and symptoms are not exclusive to Vitamin D deficiency and can be associated with other health conditions as well. If you experience any of these symptoms or suspect Vitamin D deficiency, it is recommended to consult with a healthcare professional. They can evaluate your symptoms, perform appropriate tests, and provide guidance for managing and optimizing your Vitamin D levels.
Optimizing Vitamin D Levels
Achieving and maintaining optimal Vitamin D levels requires a comprehensive approach incorporating dietary and lifestyle strategies, regular monitoring, and supplementation guided by healthcare professionals.
· Dietary Strategies: Including Vitamin D-rich foods in your diet can contribute to meeting your Vitamin D requirements. Incorporate sources such as fatty fish (salmon, sardines, mackerel), fortified dairy products, egg yolks, and mushrooms. Additionally, foods fortified with Vitamin D, such as fortified milk, cereal, and orange juice, can help boost your intake.
· Sun Exposure: Safe and sensible sun exposure is a natural way to stimulate Vitamin D synthesis in the skin. Spending approximately 15-20 minutes in the sun per day, preferably during the early morning or late afternoon without sunscreen, can support the body's production of Vitamin D. However, it is important to balance sun exposure for Vitamin D synthesis with the need for sun protection to prevent skin damage.
· Regular Monitoring: Regularly testing your Vitamin D levels through blood tests or home testing kits allows you to track your progress and ensure your levels remain within the optimal range. This monitoring provides valuable information for adjusting your dietary and lifestyle strategies or considering supplementation if necessary.
· Supplementation under Healthcare Professional Guidance: Supplementation may sometimes be necessary to achieve and maintain optimal Vitamin D levels. Healthcare professionals can assess your individual needs, consider factors such as age, health condition, and lifestyle, and guide you in selecting the appropriate Vitamin D supplement, dosage, and duration. They can also help monitor your progress and make adjustments as needed.
· Lifestyle Factors: Other lifestyle factors, such as maintaining a healthy weight, engaging in regular physical activity, and managing stress, can indirectly support optimal Vitamin D levels. These factors contribute to overall health and well-being, positively impacting Vitamin D metabolism and utilization.
Remember, optimizing Vitamin D levels is a personalized journey. Consulting with a healthcare professional is essential to assess your needs, interpret test results, and provide individualized guidance. By incorporating dietary and lifestyle strategies, regular monitoring, and appropriate supplementation, you can strive to achieve and maintain optimal Vitamin D levels for overall health and well-being.
Potential Risks and Benefits of Vitamin D Supplementation
Vitamin D supplementation can benefit individuals at risk of deficiency, such as those with limited sun exposure or specific medical conditions. However, it is important to consider the risks and benefits. Regarding vitamin D supplementation, the recommended dosage can vary depending on individual factors such as age, health condition, and specific needs. While vitamin D supplementation can be highly beneficial, it is essential to exercise caution and avoid excessive intake, as it can lead to vitamin D toxicity. Symptoms of vitamin D toxicity can include nausea, vomiting, excessive thirst, frequent urination, and kidney problems. It is important to consult with a healthcare professional who can provide personalized guidance tailored to your circumstances. They will consider your medical history, current medications, and any potential interactions or contraindications. Based on their assessment, they can recommend the appropriate dosage of vitamin D supplementation to help you optimize your levels effectively. Individualized supplementation based on blood test results and guidance from healthcare professionals is necessary to optimize vitamin D levels safely.
Conclusion
Optimizing Vitamin D levels is crucial to maintaining overall health and preventing disease. By understanding the mechanisms and functions of vitamin D, as well as the factors that affect its production and absorption, individuals can make informed decisions about sun exposure, dietary choices, and supplementation to optimize their vitamin D levels. Regular monitoring and consultation with healthcare professionals are essential for personalized guidance and support. Seeking professional help and engaging in evidence-based treatments are essential steps toward recovery. Consider taking advantage of the comprehensive healthcare services provided by Cura4U. Whether you need a lab test, consultation with a healthcare professional, or access to other medical services, Cura4U can offer a convenient and affordable solution from the comfort of your home. Our user-friendly website lets you access your test results and medical reports online, ensuring you stay informed about your health status. Always consult a healthcare professional before changing your dietary and lifestyle habits or initiating vitamin D supplementation.
Our clinical experts continually monitor the health and medical content posted on CURA4U, and we update our blogs and articles when new information becomes available. Last reviewed by Dr. Saad Zia on July 11th, 2023.
References
Vitamin D | The Nutrition Source | Harvard T.H. Chan School of Public Health- https://www.hsph.harvard.edu/nutritionsource/vitamin-d/
Vitamin D - Health Professional Fact Sheet (nih.gov)- https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/
Vitamin D Deficiency: MedlinePlus- https://medlineplus.gov/vitaminddeficiency.html
Vitamin D and Calcium | Johns Hopkins Medicine- https://www.hopkinsmedicine.org/health/wellness-and-prevention/vitamin-d-and-calcium
Vitamin D | Nutrition | CDC- https://www.cdc.gov/nutrition/infantandtoddlernutrition/vitamins-minerals/vitamin-d.html
Vitamin D supplementation and major cardiovascular events: D-Health randomised controlled trial | The BMJ- https://www.bmj.com/content/381/bmj-2023-075230
Patient education: Vitamin D deficiency (Beyond the Basics) - UpToDate- https://www.uptodate.com/contents/vitamin-d-deficiency-beyond-the-basics
Vitamin D physiology - ScienceDirect- https://www.sciencedirect.com/science/article/pii/S0079610706000083
Vitamin D: A millenium perspective - Holick - 2003 - Journal of Cellular Biochemistry - Wiley Online Library- https://onlinelibrary.wiley.com/doi/abs/10.1002/jcb.10338
Factors Influencing Vitamin D Status | Acta Dermato-Venereologica (medicaljournalssweden.se)- https://medicaljournalssweden.se/actadv/article/view/9040
Vitamin D Status: Measurement, Interpretation, and Clinical Application - ScienceDirect- https://www.sciencedirect.com/science/article/pii/S1047279708000021
Full article: Sunlight and Vitamin D (tandfonline.com)- https://www.tandfonline.com/doi/abs/10.4161/derm.24494
Vitamin D Deficiency | NEJM- https://www.nejm.org/doi/full/10.1056/nejmra070553