Multiple Sclerosis (MS) is a chronic autoimmune disease that affects the central nervous system. It is one of the most common disabling neurological conditions that affect young adults, and it can cause a wide range of symptoms that vary from person to person. MS can be difficult to diagnose, and disease management is complex and multifaceted. However, recent advances in research and medical technology have led to promising therapies that offer new hope for people living with MS.
In this blog post, we will explore the different types of MS, the causes and risk factors of the disease, its clinical presentation and symptoms, the methods of diagnosis and disease monitoring, and the available treatment options. We will also discuss the emerging therapies and treatment approaches that may offer new opportunities to personalize treatment and improve outcomes for individuals with MS.
Understanding Multiple Sclerosis: An Overview
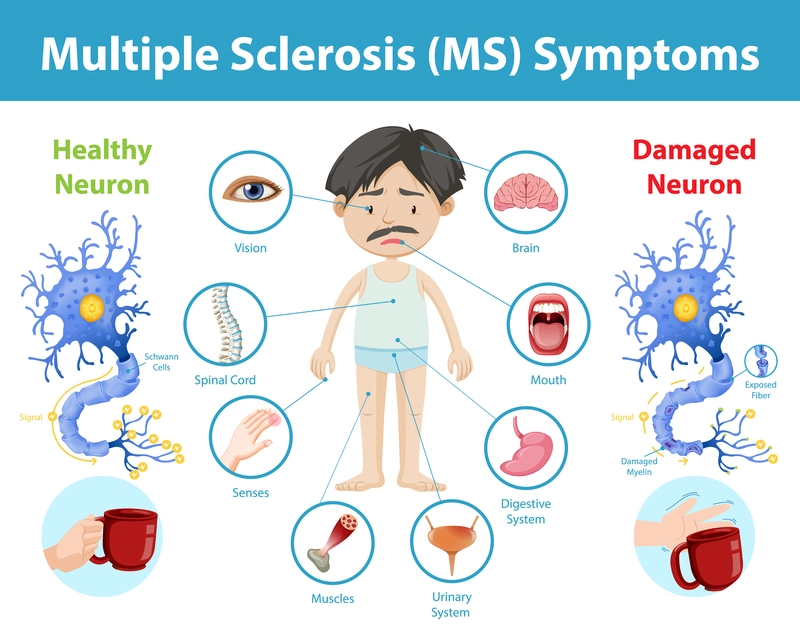
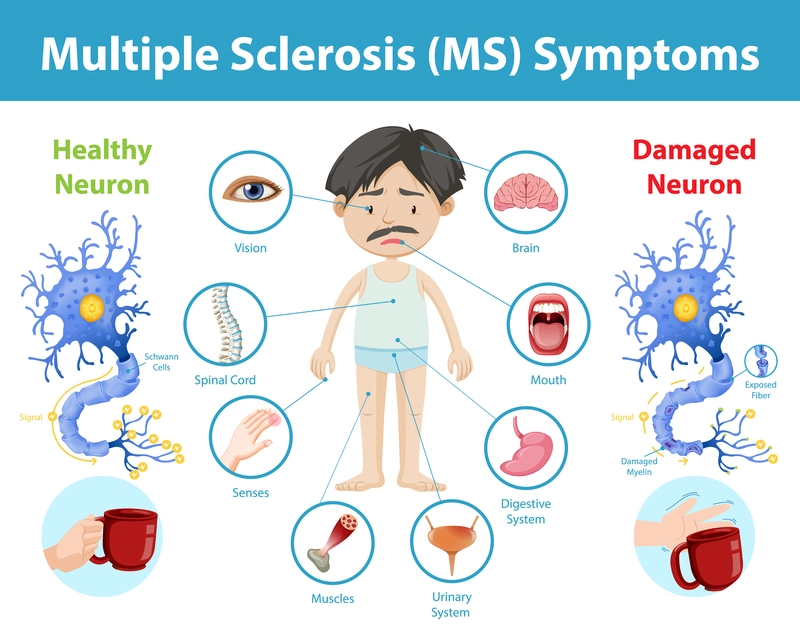
Multiple sclerosis (MS) is a chronic autoimmune disease that affects the central nervous system (CNS). It occurs when the immune system mistakenly attacks the myelin sheath, a protective covering surrounding nerve fibers in the CNS. This attack leads to inflammation and damage to the myelin, disrupting the transmission of nerve signals.
The CNS consists of the brain and spinal cord, which play crucial roles in coordinating bodily functions. When the myelin is damaged, the communication between nerve cells is impaired, resulting in a wide range of symptoms depending on the affected areas of the CNS.
Causes of Multiple Sclerosis
The exact cause of MS is not fully understood, but researchers believe it is likely due to a combination of genetic and environmental factors. Studies have shown that having a family history of MS increases the risk of developing the disease, suggesting a genetic component. Certain genes related to the immune system and the myelin sheath have been identified as potential contributors to MS susceptibility. However, genetics alone do not account for the entire risk. Environmental factors also play a role in the development of MS. Factors such as exposure to certain infections, including the Epstein-Barr virus, smoking, low levels of vitamin D, and living in regions further away from the equator, have been associated with an increased risk of developing MS.
Risk Factors of Multiple Sclerosis (MS)
In addition to genetic and environmental factors, several risk factors have been identified in relation to MS. Women are about two to three times more likely to develop MS compared to men, suggesting a gender-based risk factor. The disease most commonly begins between the ages of 20 and 40, indicating that young adulthood is a period of increased susceptibility. People of certain ethnic backgrounds, such as Northern European descent, have a higher risk of developing MS. Moreover, individuals who have experienced certain viral infections, such as the Epstein-Barr virus, are more prone to developing MS. Smoking has also been identified as a risk factor, as smokers are more likely to develop the disease than non-smokers. Furthermore, lower vitamin D levels, which can result from limited sunlight exposure or inadequate dietary intake, have been associated with an increased risk of developing MS.
It's important to note that while these factors are associated with an increased risk of MS, they do not guarantee the development of the disease. Additionally, other factors may be involved in the complex interplay of genetics, environment, and individual susceptibility to MS.
Types of Multiple Sclerosis
There are four main types of multiple sclerosis, each characterized by different patterns of disease progression:
- Relapsing-remitting MS (RRMS): This is the most common type of MS, characterized by episodes of new or worsening symptoms followed by periods of remission. During remission, symptoms may partially or completely disappear.
- Secondary progressive MS (SPMS): After an initial period of relapsing-remitting MS, some individuals transition to secondary progressive MS. In SPMS, there is a gradual and steady worsening of symptoms, with or without periods of relapse.
- Primary progressive MS (PPMS): PPMS is characterized by a steady worsening of symptoms from the onset of the disease, without distinct relapses or remissions.
- Progressive relapsing MS (PRMS): This is the least common type of MS, characterized by a steady worsening of symptoms, with occasional relapses and no periods of remission.
Identifying the Symptoms and Clinical Presentation of Multiple Sclerosis (MS)
Multiple Sclerosis (MS) is a complex neurological condition characterized by a wide range of symptoms, which can vary among individuals based on the location and extent of damage in the central nervous system (CNS). Recognizing these symptoms is crucial for early detection and management of the condition. Here are some common symptoms experienced by individuals with MS:
- Muscle weakness or stiffness: MS can lead to muscle weakness or stiffness, affecting mobility and coordination. This may result in difficulty walking or performing daily tasks.
- Numbness or tingling: Many individuals with MS experience numbness or tingling, commonly felt in the arms, legs, or face. These abnormal sensations may come and go or persist for extended periods.
- Tremors: Involuntary shaking movements, particularly in the hands, can be observed in individuals with MS. These tremors can impact fine motor skills and dexterity.
- Fatigue: MS-related fatigue is a prominent symptom characterized by a profound sense of tiredness and a lack of energy. It can be debilitating and interfere with daily activities.
- Problems with coordination or balance: MS can affect the cerebellum, leading to difficulties in coordination and balance. This may result in unsteady walking or a feeling of instability.
- Difficulty with vision: Visual problems are common in MS and can manifest as blurred vision, double vision, or even a complete loss of vision in one eye. Optic neuritis, inflammation of the optic nerve, is often associated with MS and contributes to visual disturbances.
- Cognitive impairment: Some individuals with MS experience cognitive difficulties, including problems with memory, attention, and problem-solving. These cognitive impairments can significantly impact daily functioning and quality of life.
It's important to emphasize that not every person with MS will experience all these symptoms, and the severity and progression of symptoms can vary widely. If you or someone you know is exhibiting any of these symptoms, it is crucial to consult a healthcare professional for an accurate diagnosis and appropriate management strategies. Early intervention and treatment can help alleviate symptoms and improve the overall quality of life for individuals living with MS.
Diagnosis and Disease Monitoring of Multiple Sclerosis (MS)
Diagnosing multiple sclerosis (MS) can be challenging due to the absence of a single definitive test. Instead, a comprehensive diagnostic process typically involves a combination of clinical evaluation, neurological examinations, and diagnostic tests. These tests are crucial for reaching an accurate MS diagnosis and ensuring appropriate management. Several commonly used diagnostic tools aid in the diagnostic process:
- Magnetic resonance imaging (MRI): This non-invasive imaging technique is instrumental in detecting areas of inflammation and damage in the central nervous system (CNS). By providing detailed images of the brain and spinal cord, MRI helps support the diagnosis of MS by revealing characteristic lesions or plaques that indicate ongoing disease activity.
- Lumbar puncture (spinal tap): This procedure involves the collection of cerebrospinal fluid (CSF) through a needle inserted into the lower back. The CSF is then analyzed for specific markers, such as oligoclonal bands and elevated immunoglobulin levels, which can provide evidence of immune system activity in the CNS. These markers can support the diagnosis of MS and differentiate it from other neurological conditions.
- Evoked potential tests: These tests evaluate the speed and strength of electrical signals generated by the brain in response to sensory stimuli, such as visual, auditory, or sensory inputs. By measuring the brain's electrical activity, evoked potential tests can help identify abnormalities in nerve pathways, which may indicate impaired transmission caused by MS-related damage.
Once an individual receives an MS diagnosis, regular disease monitoring becomes essential. This monitoring allows healthcare professionals to assess disease progression, evaluate the effectiveness of treatments, and make any necessary adjustments to the management plan. Regular neurological examinations, imaging studies (such as follow-up MRIs), and clinical evaluations help track changes in symptoms, identify new disease activity, and guide treatment decisions to optimize long-term outcomes for individuals with MS.
By employing a combination of clinical evaluation, neurological examinations, and various diagnostic tests like MRI, lumbar puncture, and evoked potential tests, healthcare professionals can accurately diagnose MS and implement appropriate disease management strategies. Continuous monitoring ensures ongoing assessment and adjustment of the treatment plan to address the individual needs of people living with MS effectively.
Current Treatment Approaches of Multiple Sclerosis (MS)
While there is currently no cure for multiple sclerosis (MS), a range of treatment approaches is available to effectively manage symptoms, slow down disease progression, and improve the quality of life for individuals living with MS. These treatment options encompass various aspects of care:
- Medications: Disease-modifying therapies (DMTs) play a central role in managing MS. These medications aim to reduce inflammation, modify the immune response, and slow down the progression of the disease. DMTs include injectable therapies such as interferons, glatiramer acetate, and oral medications like fingolimod and teriflunomide. Other more targeted and newer medications are also available, providing a wider range of options for personalized treatment plans.
- Rehabilitation therapy: Rehabilitation therapy, including occupational therapy, physical therapy, and speech therapy, plays a vital role in helping individuals with MS improve their overall functioning and quality of life. Occupational therapy focuses on assisting individuals in managing daily activities, adapting to limitations, and maximizing independence. Physical therapy helps improve mobility, strength, and balance, while speech therapy addresses any speech or swallowing difficulties that may arise.
- Lifestyle modifications: Certain lifestyle modifications can significantly contribute to managing MS symptoms and overall well-being. Regular exercise tailored to individual abilities and preferences can help improve strength, flexibility, and overall fitness. A balanced diet with essential nutrients, such as omega-3 fatty acids, vitamins, and minerals, supports general health. Stress reduction techniques, such as mindfulness, meditation, or relaxation exercises, can help individuals cope with the emotional and physical challenges of living with MS. Additionally, ensuring adequate rest and quality sleep are essential for managing fatigue and optimizing overall health.
Individuals with MS must work closely with their healthcare team to develop a comprehensive treatment plan that addresses their needs. Treatment approaches may vary depending on the type and severity of the disease, as well as individual preferences and responses to therapy. Regular monitoring and follow-up with healthcare professionals are crucial to assess treatment effectiveness, adjust therapies if necessary, and ensure optimal management of MS over time.
Ongoing research and advancements in treatment options continue to offer hope for improved outcomes and quality of life for individuals with MS.
Emerging Therapies and Treatment Approaches of Multiple Sclerosis (MS)
Multiple sclerosis (MS) research is witnessing exciting advancements, paving the way for developing new and promising treatment approaches. These emerging therapies offer hope for enhanced management and improved outcomes for individuals with MS. Some notable emerging treatment approaches include:
- Novel medications: Researchers are actively developing medications targeting different disease aspects. These novel medications reduce inflammation, promote myelin repair, and protect nerve cells. By specifically addressing these key factors, they have the potential to slow down disease progression and alleviate symptoms associated with MS.
- Targeted immunotherapies: Targeted immunotherapies represent a promising approach to MS treatment. These therapies focus on modulating the immune response by targeting specific immune cells or receptors involved in the development and progression of MS. By precisely influencing the immune system. These therapies aim to restore balance and prevent immune-mediated damage to the central nervous system.
- Stem cell transplantation: Stem cell therapy is an emerging research area with tremendous potential for MS treatment. This approach involves replacing or repairing damaged cells in the central nervous system by introducing healthy stem cells that can differentiate into various cell types. Stem cell transplantation can promote myelin repair, reduce inflammation, and restore normal functioning in the affected areas.
- Precision medicine approaches: Advances in genetics and personalized medicine have opened up new avenues for predicting and treating MS. Precision medicine considers an individual's unique genetic profile and disease characteristics to tailor treatment decisions. By identifying specific genetic markers or disease factors, healthcare professionals can customize treatment plans, optimizing their effectiveness and minimizing potential side effects.
These emerging therapies and treatment approaches are still undergoing rigorous research and clinical trials. While they hold promise, it is important to recognize that their full effectiveness and safety profiles are yet to be fully established. Individuals with MS must consult with their healthcare providers to stay updated on the latest advancements and determine the most appropriate treatment options based on their specific circumstances.
As the field of MS research continues to advance, developing these novel treatment approaches brings hope for more targeted and effective interventions. With further scientific breakthroughs, personalized and precise therapies have the potential to revolutionize MS treatment, leading to improved outcomes and a better quality of life for individuals living with this complex neurological condition.
Conclusion
In conclusion, multiple sclerosis (MS) is a complex condition that affects the central nervous system and requires a comprehensive approach to management. While there is no cure for MS, various treatment options, including medications, rehabilitation therapy, and lifestyle modifications, can help manage symptoms and slow disease progression. Exciting advancements in MS research are leading to emerging therapies, such as novel medications, targeted immunotherapies, stem cell transplantation, and precision medicine approaches. These offer new hope for more effective and personalized treatment. At Cura4U's NeuroX clinic, we provide comprehensive counseling and mental health services to support individuals with MS. Prioritizing mental health, seeking help, and reducing stigma is crucial for overall well-being. We are here to assist you on your journey to better mental health, as we believe that your well-being matters.
Our clinical experts continually monitor the health and medical content posted on CURA4U, and we update our blogs and articles when new information becomes available. Last reviewed by Dr. Tayyab Saeed Akhter on July 4th, 2023.
References
Multiple sclerosis - NHS (www.nhs.uk)- https://www.nhs.uk/conditions/multiple-sclerosis/#:~:text=Multiple%20sclerosis%20(MS)%20is%20a,it%20can%20occasionally%20be%20mild
Multiple Sclerosis (MS) | Johns Hopkins Medicine- https://www.hopkinsmedicine.org/health/conditions-and-diseases/multiple-sclerosis-ms
What is MS? | National Multiple Sclerosis Society (nationalmssociety.org)- https://www.nationalmssociety.org/What-is-MS
Multiple Sclerosis | National Institute of Neurological Disorders and Stroke (nih.gov)- https://www.ninds.nih.gov/health-information/disorders/multiple-sclerosis
Multiple Sclerosis: Practice Essentials, Background, Pathophysiology (medscape.com)- https://emedicine.medscape.com/article/1146199-overview
Multiple Sclerosis: What Is MS? Overview, Risk Factors & Outlook (webmd.com)- https://www.webmd.com/multiple-sclerosis/what-is-multiple-sclerosis
Multiple Sclerosis: Pathogenesis, Symptoms, Diagnoses and Cell-Based Therapy - PMC (nih.gov)- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5241505/
Multiple sclerosis – a review - Dobson - 2019 - European Journal of Neurology - Wiley Online Library- https://onlinelibrary.wiley.com/doi/abs/10.1111/Ene.13819
Multiple Sclerosis (saudedireta.com.br)- https://www.saudedireta.com.br/docsupload/1421610595p712.pdf
Multiple sclerosis: clinical aspects : Current Opinion in Neurology (lww.com)- https://journals.lww.com/co-neurology/Fulltext/2018/12000/Multiple_sclerosis__clinical_aspects.15.aspx
Current and emerging treatment of multiple sclerosis. - Abstract - Europe PMC- https://europepmc.org/article/med/27356025